Someone reached out to me on Facebook last month and asked if I had retired. “What gave you that idea?” I responded. She remarked that she couldn’t understand how I could be still working if I was hiking so much around the world. “Well, first off, I don’t have kids. What’s that joke? If you have a shit job but no kids, you are rich. If you have a high paying job but you have kids, you’re poor. Ha. But no, I’m not retired. I just figured out what pays the most in 21st century America.”
“What’s that?”
“Politics.”
I could tell you more about the conversation, about how she was upset that I was working for both Republicans and Democrats. And how I responded that it would be stupid to cut off half my potential clients. I could spell out exactly how she questioned my principles and how she was outraged when I asked her what country she lives in. But I think you get the point. So I’m just going to share with you a snippet of a conversation that occurred in a Southern Republican Governor’s Mansion from late January after I had completed my Winter 46 in the Adirondacks. I’ll put it in the form of a play. I am the consultant (TC). The Governor is (GOV). Bob (B) is the Governor’s chief of staff and Kate (K) is my assistant.
GOV: Thanks for coming down.
TC: Well the check was convincing.
GOV: Ha. How was your flight?
TC: Terrible. We had to connect in Atlanta.
GOV: Sorry.
TC: Not your fault. But if you get elected, you’ve got to make it so people can get a direct flight from New Jersey to your state capitol. You know, everyone agrees that if you can’t fly somewhere directly from Newark, it’s not a serious place.
B: (stepping in to break the tension) Ahem. We really do appreciate you coming down here. And you are right…there should be a direct flight from both New York and DC to the capitol. Something for us to work on with the airlines.
K: (jumping in) Just give them a tax break. They’ll do whatever you ask.
GOV: (smiles, looks to Bob) See, this why we brought them down.
B: Can you tell us about some of your policy plans that can up the Governor’s profile?
TC: Of course. There are three things that you can start doing in your state today. Job creation through international prisons. Freedom and child protection through guns in schools. Cost savings by cutting lazy public workers’ salaries, benefits and pensions. All three of these will put you at the center of the political world. Republican votes will love it, liberal pansies will hate it, and everyone fucking cable news channel will talk about it. Win, win, win.
B: Interesting. Let’s start with international prisons.
TC: As you are painfully aware, two of the federal prisons in your state closed because of the Obama administration.
K (sees GOV and B shift uneasily and jumps in): We know that Obama’s soft criminal justice policies caused the economic meltdowns in both Madison and Springfield. Frank is suggesting that you reopen those prisons immediately.
GOV: How would we do that?
TC: Who does prisons better than the United States? (pause). No one. We’re the best. And I have to say, your state has an amazing track record when it comes to incarcerating her citizens. Now we have these empty prisons and all of these highly skilled correction officers out of work. What I suggest is that we let the world know that they can send their prisoners here. To your state. You’ll house them, feed them, cloth them and put them to work.
K: For the more repressive states, we’ll play down the “house them and feed them” parts and play up the “punishment” parts.
TC: That was Kate’s insight. She’s very smart.
GOV: (smiling) Clearly.
TC: Obviously some countries are richer than others. But everyone has to pay the same rate.
B: (getting in the mood) After all, we aren’t fucking communists.
TC: Exactly Bob, exactly. We aren’t fucking communists. So the countries that can’t pay as much need to pony up some political support for you Greg.
GOV: What does that look like?
TC: Ha. I don’t know. But think of it like “The Godfather.” Some day you may need a favor, and that day may never come, but if it does, Cambodia needs to step the fuck up.
GOV: Fantastic.
TC: Anyway, you’ll get paid for every prisoner, get some political support and you’ll immediately create 2500 jobs in Madison and Springfield. You’ll bring those towns back. Obama destroyed those towns. You Greg, fucking saved them.
K: And once you do it here, if you are elected President, you could do it in other states.
GOV: Jesus. We don’t need to hear anymore. You’re hired. When can you come aboard?
TC: Greg. Thank you. (puts his hands in prayer). Thank you. But I really want to talk to you about the other two proposals. Remember, this is a three part plan.
GOV: (giddy, like a child) Ok, ok.
TC: There are so many school shootings. Kids dying everywhere. Those pussies in Texas just sat there as kids got murdered. The DC politicians do nothing. Bush did nothing. Obama did nothing. Trump did nothing. Biden has done nothing. You can solve it. Do you want to solve it Greg?
GOV: I do, I really do.
TC: Does he want to solve it Bob?
B: He does, he really does.
TC: Kate?
K: Thanks Frank. You are going to arm the children.
B: What?!?
GOV: Hold on Bob, let her speak.
K: Boys in first grade up can carry rifles. Boys in fifth grade can carry handguns. Girls in fifth grade get rifles and girls in eighth grade can have handguns.
GOV: (looking at the TC) Why do boys get guns earlier than girls?
TC: Kate?
K: (not missing beat) Females are too emotional.
B: Wait a second. Why are we doing this?
TC: To stop school shootings Bob.
B: Well, excuse me for asking, but what happens if a kid shoots another kid. The Governor will be flayed.
TC: Bob, you are sounding very weak on the 2nd Amendment right now. Are we going to be able to keep you on? (the Governor and Kate both look at him)
B: (stuttering) Well, what happens if a kid shoots someone who isn’t a school shooter? Are we going to punish the kids?
TC: Well, no. We aren’t going to punish children. Jesus, Greg, what is with this guy? The kids will be put on a 30 day gun time out. And then they’ll have to do some remedial training.
K: We’ll punish their parents for not teaching them proper restraint. Some of them will need to go to prison, which will help us reopen the state prison that closed in Bakersville last year.
TC: Look Greg, I know this one is controversial, but it is going to make Twitter explode. You are going to be on the cover of Time.
K: (stands up and takes a fake issue of Time with the Governor on the cover) “The Most Dangerous Man in America or The Next President.”
TC: And when people ask that, you know what you fucking say Greg?
GOV: No, what do I say?
TC: Both. “I’m the most dangerous fucking man in America and the next President.”
B: I don’t know….
GOV: Not another word Bob.
TC: Last one. We’re going to cut teachers salaries and pensions immediately.
GOV: Their unions won’t go for it.
TC: Those liberal teachers unions? Who only back Democrats? Who cares? You put it on a ballot.
K: A special referendum. So important it is held next month. This won’t give them a chance to organize or get their messaging out. Meanwhile, you just play up how the teachers groom kids to become bi-sexual, make them read books that put down white people and basically don’t teach them anything. Bob, you have kids. What did your kids learn on Zoom during COVID?
B: (happy to be included again) Not much.
K: (saying it slowly) Not much. Exactly Bob. So, Governor, what are these teachers actually doing?
GOV: I don’t know.
K: Exactly. And we don’t pay for I don’t know. So we’ll leave it up to the voters to cut their pay.
B: How will we attract new teachers if their pay is low and they have no pensions?
K: We’ll offer them free iPhones and super strong cannabis.
GOV: Do you think they’ll go for that?
K: Generation Z is incredibly stupid. They’ll do almost anything for weed and iPhones.
TC: But we aren’t only going to cut teacher’s salaries. We are going to cut law enforcement salaries and their pensions too.
GOV: Our voters love the police. They won’t go for it.
TC: Well, that’s why we aren’t going to put it to a vote. We’ll let the cops do it to themselves.
B: How?
TC: The older cops will vote for lower salaries and pension reform, we don’t call it elimination, we call it reform. Anyway, the older cops will push it through if we give them a little bonus and a few extra days off.
GOV: Won’t it seem like we are buying them off?
TC: Greg, don’t be so naive. With all the budget cuts in the newspapers down here, there are no state house reporters to be found. You’ll let the older cops know about the bonus and time off through back channels. The public will never hear about it. All they’ll know is that their genius Governor got the cops to lower their own salaries and save the tax payers a whole heap of money.
B: Amazing. I had my doubts about this, but your plan is fantastic.
K: Thank you Bob.
B: What about our rivals in the primary?
TC: Nikki Haley.
K: A woman. Ha. Republican voters aren’t electing a female President.
TC: Unless her last name is Greene. (pause, everyone nods).
GOV: Pence?
Everyone: Hahahahahaha.
Bob: DeSantis.
TC: Well, Ron has a fucking true genius on his staff. Going after children’s books and immigrants and Disney was brilliant. Kate is going to find out which staff member proposed those ideas and try to lure him into our camp.
B: What about his military service?
TC: We can beat up Ron on his military service.
K: We can plant a rumor that maybe he blew a general to get promoted. We can make it appear like it came from Trump’s team.
GOV: I don’t know if the public will go for attacking someone’s service.
TC: Greg, hello? John Kerry was destroyed for his service in Vietnam. Trump shit all over McCain’s imprisonment and the primary voters loved him for it. Fuck Ron’s service. Fuck any opponent’s military service.
B: That’s all well and good, but how do we defeat Trump in the primary?
TC: Well, it’s a longshot. If we defeat him, great. But if you lose, we’ll have drawn so much blood that he can’t win. Then you’ll be the heir apparent in 2028.
GOV: How do we bloody him up? Nothing seems to stick.
TC: Kate?
K: A vote for Trump is a vote for Biden. (silence)
B: What does that even mean?
TC: It means they are both criminals. Take every chance to tie Trump to Biden.
B: That’s crazy. Trump criticizes Biden all the time.
K: Just keep saying they are buddies. Part of the same DC cabal. “A vote for Trump is a vote for Biden.”
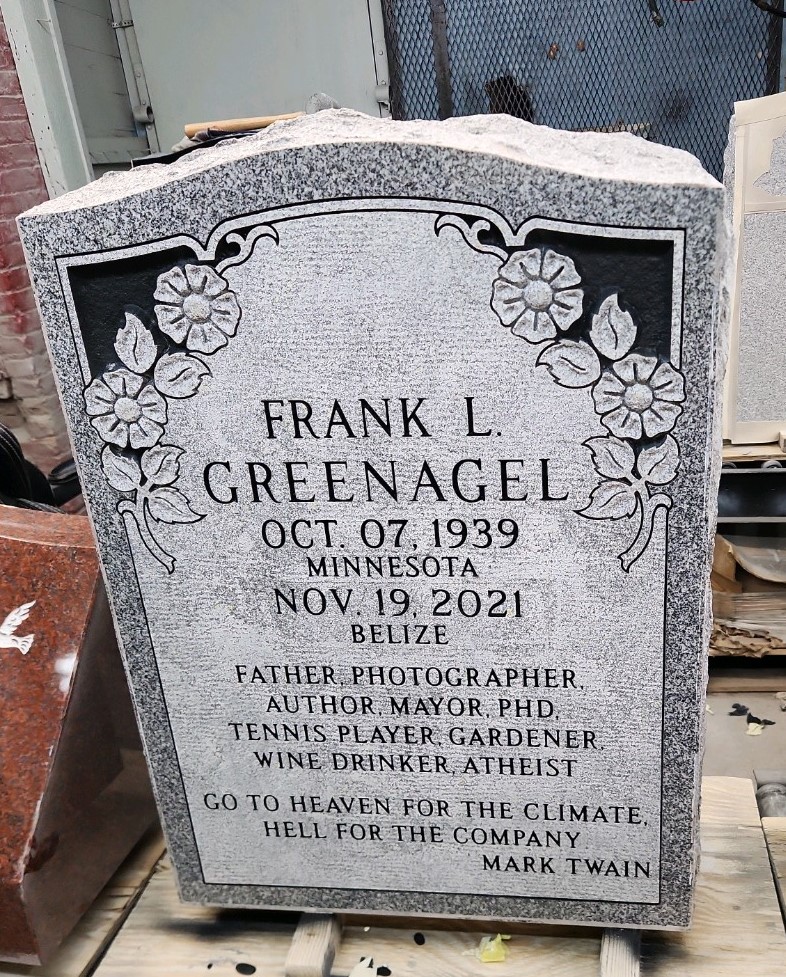
* I want to thank Jonathan Swift, Mark Twain, and Jon Stewart for the spiritual inspiration for this piece. If you haven’t figured it out yet, please check the date.